Twin Talks
Inside the NICU: Transitioning Twins to Home
[00:00:00]
Please be advised, this transcription was performed from a company independent of New Mommy Media, LLC. As such, translation was required which may alter the accuracy of the transcription.
[Theme Music]
CHRISTINE STEWART-FITZGERALD: If you have twins in the NICU, one of the biggest questions is: when can I take them home? And then once you have an idea of when you can take home one or both of them, the next question is: How will we make that transition from a highly equipped facility that is staffed 24/7 by an expert team of nurses to our home that is staffed by often overwhelmed parents? How should we set up the nursery? Should we try to keep them on the same schedule as in the NICU? Do we need any special equipment? This is Twin Talks.
[Intro/Theme Music]
CHRISTINE STEWART-FITZGERALD: Welcome to Twin Talks broadcasting from the Birth Education Center of San Diego. Twin Talks is your weekly online, on the go support group for expecting and new parents of twins. I’m your host, Christine Stewart-Fitzgerald. Have you heard about the Twin Talks Club? Our members get bonus content after each new show plus special giveaways and discounts.
Subscribe to our monthly Twin Talks newsletter and learn about the latest episodes available. And another way for you to stay connected is by downloading our free Twin Talks app. It’s available in the Android and iTunes market place.
Before we get started, let’s introduce our panelist. I’m going to start with our panelist on the phone today. Julie, can you share a little bit about your family and maybe a little bit about your NICU experience.
JULIE KREMRAI: I’m Julie Kremrai. I’m 49. About to—I’ma CPA. I have twin girls who are now six years old.
CHRISTINE STEWART-FITZGERALD: And let’s see, Suzie.
SUZIE DEGWENN: Hi there. I’m Suzie Degwenn. I’m 44 years old. I’m a provider relationsliaison for Steward Fitness Program. I have four children. One boy, Christian. And just three months ago, had triplets two boys, Gideon and Gabriel and a girl, Charlotte.
CHRISTINE STEWART-FITZGERALD: Wow.
SUNNY GAULT: I know. That’s kids.
CHRISTINE STEWART-FITZGERALD: And let’s see, I’m your host, Chrisitine Stewart-Fritzgerald and I’ve got my girls-my twin girls are identical and they’ve just turned six years old. One of them spent just a few hours in the NICU so I don’t think I can really make any claim to having any experience there. I do have a singleton, who just turned three years old and I think she’s the one. She runs the show.
SUNNY GAULT: And I’m Sunny. I’m producing today’s show and I have four kiddos of my own. A five year old boy, three year old boy and I have identical girls who are turning two next week. They were 35-weekers. In my mind, I was like: “I’ve got to get to 35. I’ve got to get to 35”. I think I tricked my body into naturally going into labor because I was 35 weeks and two days when one of my babies broke her water and when I went into labor. But they didn’t need NICU experience at all. They didn’t need it and we were able to go home within a few days so, thankfully.
CHRISTINE STEWART-FITZGERALD: Oh awesome. Sunny can you tell us something about getting involved with the show?
SUNNY GAULT: Yes. We’d love hearing from our listeners. We have these segments that we want you guys can participate in because we’d love to hear just your funny stories of raising twins and the cool things your twinnies are doing. There’s a couple that I wanted to mention. We have a segment called Special Twin Moments. As you guys know as twin parents, sometimes your kids just do these awesome things that you just want to remember forever. And we want to hear about those.
We’ve heard some cute stories of twins cuddling together. We’ve actually—a lot of people submitted photos, which is great because I love looking at them but I can’t really show them to you guys because this is an audio podcast. So we want to hear these actual great stories that you’ve experienced with your twins.
There’s another segment called Twin Oops. We all make mistakes when it comes to raising twins and stuff and sometimes these mistakes are pretty darn funny and definitely would help if other twin parents heard it and just need it. We’re all parents. We all make mistakes and its all good kind of thing.
We have a bunch more segments and you can check them out on our website at www.newmommymedia.com. Just go over to the Twin Talks section. But if you want to submit to any of our segments, again through our website, go to the contact link and you could kind of type it out there.
If you actually want to share your story yourself, as opposed to me or Christine reading it, you can call our voicemail and that number is 619-8664775 and then you’ll go straight to voicemail. Just leave your message and we’ll include it in an upcoming episode.
[Theme Music]
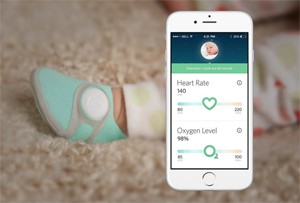
SUNNY GAULT: Hey Twin Talks. Before we start today’s episode featuring NICU parents and their tips for transitioning their babies to living at home, we are going to chat with our friends at Owlet because they’ve created the Owlet Smart Sock. I had the chance to check it out first-hand recently at the ABC Kids Expo and I really think it can help NICU parents ensure their babies are safe once they come home. Kurt Workman is the CEO and he’s joining us today. Hi Kurt and welcome to Twin Talks.
KURT WORKMAN: Hi Sunny. Thank you so much for having me. I’m really excited to talk about the product.
SUNNY GAULT: Yes. So you guys have created a monitor that fits inside a baby bootie. I want to kind of have a visual on this. How exactly does the Owlet work?
KURT WORKMAN: That’s right. We have—it’s almost as simple as that you put the little baby bootie on a night, it slips around the foot and Velcro’s around the heel so it doesn’t fall off. It’s comfortable. It uses organic cotton. The monitor itself inside the baby bootie, it tracks the baby’s heart rate, and oxygen levels and sends all that information to mom and dad’s smart phone. It can actually alert them if the heart rate or oxygen is too high or too low.
SUNNY GAULT: So we’re focused on oxygen and heart rate. Those are the vital signs the parents can monitor then from their smartphones?
KURT WORKMAN: Yes. That’s correct. It’s really kind of in correlation to breathing. It’s designed to alert parents if the baby stops breathing at night.
SUNNY GAULT: Even though we are trying to get parents to look at these vital signs; to be aware of what their baby’s vital signs should be, the other goal is to just let parents kind of step back and relax. Not always staring at vital signs, right?
KURT WORKMAN: Oh absolutely. Yes. It’s definitely not an obsessive product. In fact, overtime, parents kind of put the app away and they just trust that they will get a notification or get an alert if something is wrong. So that’s why we’ve developed this little—called the base station that goes into mom and dad’s night stand.
It glows based on the status of baby. When everything’s good, that base station will glow green. If there’s a problem it flashes red and sounds an alarm. What we see is that over time, parents realize, hey this actually works and I don’t have to be hovering over the app.
The data ran out, the data obsessed company and really about adding reassurance and peace of mind and kind of removing that kind of worry from home so mom and dad can be in the moment with their child.
SUNNY GAULT: I have to ask. How did the product come about? Was this something that you had some personal experience with or someone within the company?
KURT WORKMAN: That’s a great question. Two and a half years ago—my son is two years old now. Two and a half years ago we were expecting our son, Ashton, and my wife has congenital heart defect so she’s had multiple heart surgeries. When she came home from the hospital, they didn’t diagnose it. We ended up rushing her back to the hospital. She had a heart surgery that day. That’s a story that just really stuck in our mind.
With our kids, with our son—we’ve got another one on the way, it’s due in February. With her we’ve also been doing all these fetal heart echo’s to make sure that the heart is healthy because that can be hereditary. We’re doing these fetal heart echo’s—as a future dad, I’m really concerned that something could happen. I had that kind of heightened awareness.
At the same time, we’re helping my aunt with her premature twins. And have all our nieces and nephews. We’re just pretty much thinking about this. Then my friend, Taynor came to me and he said, “hey, I have this idea for this technology called pulse oximetry which is a little light which can monitor heart rate and oxygen levels. “ I just became fascinated with the idea that maybe we can make this technology appropriate for the home and give parents access to that technology in a way that’s reassuring and also very informative. Because I know it’s something that I would want.
My experience is one with these emails from parents who are just really begging for some sort of a prototype of this concept so we decided to just dive into it. We’ve quit our jobs. We didn’t take a salary for the first year. We’ve been working on it for two and a half years now and just kind of dedicated our lives to being hailed at to bring this into the home and we think while we increase health and safety to the home.
SUNNY GAULT: Well Kurt, we really appreciate you creating this product. I know it’s not easy to do especially when you have a young family. There’s a lot of moving parts there. It was important enough for you to get it out there to the public. I’m sure I’m not the only person—there are a lot of families out there that thank you for working on this technology and making it available for parents. Thanks so much for doing that.
We want to let all of our listeners know that Owlet is offering free shipping within the continent of United States, through the end of 2015. And that’s when you purchase on their website which is www.owletcare.com. We’re going ahead and link them directly to our website. You can just head over to www.newmommymedia.com and click on the Deals Section.
Kurt, again, thank you so much for being with us today. We really appreciate your time.
KURT WORKMAN: Thanks so much Sunny.
[Theme Music]
CHRISTINE STEWART-FITZGERALD: We are here today, continuing our series: Inside the NICU. We’re talking with our expert parents who are sharing their tips on the practicalities of bringing home twins from the NICU. Thanks for joining us Suzie and Julie. Give us some perspective on- we want to hear what your experience was with the NICU. How long were your babies in the NICU? Suzie, we’ll start with you.
SUZIE DEGWENN: My babies were 30-weekers. My boys stayed in the NICU for 59 days. I’m laughing as I tell you this because I thought “I’ll estimate it, I’ll say months or weeks”. You’ll definitely countdown every single day. So anyhow, 59 days then I had to leave my little girl in the NICU for an extra week. She clocked 66 days.
CHRISTINE STEWART-FITZGERALD: Wow, so about a week after your boys.
SUZIE DEGWENN: Yes and it was really hard to—I wasn’t necessarily expecting to feel that kind of disappointment and sadness. I was so excited about taking the boys home. And then, it kind of hit me—I have to leave her.
CHRISTINE STEWART-FITZGERALD: Wow. That’s hard. And we’re going to talk about that idea of having one in and some at home. Julie, how about you? Tell me about your girls. How long were they in the NICU?
JULIE KREMRAI: My girls were born at 30 weeks and zero days. Skyler was 2lb and 15oz. She was in the NICU for exactly seven weeks which was exactly 49 days. Kennedy being 1lb 15 oz. She stayed in the NICU for 75 days, which is two days short of 11 weeks. This actually brought up all kinds of emotions during that time. It was very hard. Very, very hard.
CHRISTINE STEWART-FITZGERALD: I have to say, as I listen to both of you talk about how many days—sounds like everyday you were very, very cognizant of how much time and literally just counting down. I’m wondering when they were born or any point during their stay, did you feel like you had a clear idea of what to expect in terms of their stay? Or were there changes? What was that like for you? Julie?
JULIE KREMRAI: To be honest with you, when I was pregnant—early on—I was reading one of those guide books about what to expect in the pregnancy and how to raise them and all that and I was 43 years old. I was reading this one part which was about women around my age only had 8% chance of getting pregnant and 4% chance to live birth. And I immediately closed the book and I did not read anything anymore. Which is kind of opposite from my personality who must do research and everything.
So the point is I was pretty clueless of what to expect in terms of being pregnant, giving birth, and I certainly knew absolutely nothing about NICU. I think in a way it was good because not knowing so much, I just followed the lead of the nurses and the doctors instead of questioning them and everything that they do, whether they were doing the best for my babies. In one word, I was clueless.
CHRISTINE STEWART-FITZGERALD: So maybe what you’re saying is, in some way, not having a whole lot of expectation was probably a good thing because then you weren’t disappointed by not meeting some book guidelines that were out there. Suzie, how about you? Did you have any kind of set expectations, going into it all?
SUZIE DEGWENN: Julie, I would try to be more like you. To me, knowledge is comforting so when you’re in that scary situation—one of the first things that I asked the doctor, the neonatologist was: “Okay, they’re 30-weekers. When do they get to go home?” Depending on who you speak to, you get a different answer. Some folks said, “hey, you’re going to be—your singleton due date, give or take a couple of weeks”. Probably the best answer I got was: try not to have that arbitrary date on the calendar because your baby is in the driver’s seat. She’s going to tell us when they’re ready to go home. That was something I could wrap my head around.
I did have expectations though, going into the NICU because I asked other parents. I knew I had plenty babies, they’re triplets. I asked a lot of other parents. I knew about the terminologies, I knew about the bells from the monitors, kind of what the environment would be like.
I’ll tell you, one thing that I was not prepared for and this was my bad. I spoke with a lot of singleton parents. I wish I would have spoken with more twin or triplet-moms. That’s simply because I wasn’t prepared to have a really, really good day with one baby then I’d walk over to the other baby and it was a really, really bad day. Something that I learned in that couple of months was if there was a good rapport, good rapport means they jumped hurdles, that they were all stable and doing well. If you have good rapport with all three, I really celebrated that.
CHRISTINE STEWART-FITZGERALD: You bring about an excellent point. We’re talking about twins when they are older and we have all these ideasthat they should all be the same. I think you’re pointing out that even when they’re in the NICU, their health and development is going to be different and so we have to keep that mindset that they are individuals, and have different expectations for each of them. For each of you, did your receive any kind of training or instructions from the NICU team about what to expect when you were able to take them home? I think you mentioned you connect with parents. Did you get any tips and tricks from other parents as well? Suzie?
SUZIE DEGWENN: Specific to that transition home, every NICU is different. But our NICU actually offered an opportunity to room-in with the babies the night before they were going home. Essentially what that means is they are still connected to all of their monitors. You’re just in a hospital room with those babies or baby. And you’re getting to do their care for them—all of the feedings changing their diaper, pinning them down the rest, that kind of thing. That was very comforting to me. It was almost like a dress rehearsal or a trial run so to speak.
I mentioned earlier that my first discharge was those boys at once. Having been a parent to a singleton two years prior to this, that was definitely when I knew for the first time that more than one baby was a totally different ball game. One of my sons—we have been joking for weeks—he’s so laid back, he’s so chill. And then I learned in that overnight room-in, no, he’s not so laid back and chill.
We just think his nights are his days. That was the first time that we figured that out. When I compared notes with the night nurses versus the day nurses, they said, “oh he’s not laid back at all. He’s a party animal.” But I had that dress rehearsal to learn that before I brought them home.
CHRISTINE STEWART-FITZGERALD: Wow, that’s interesting. So you get that perspective that maybe you have not had before to see the night time since you hadn’t really spent time with them atbefore. Was that similar on your experience, Julie, as well? What sort of ready-to-go instructions did you get?
JULIE KREMRAI: I think it was just not ready-to-go because I was learning from the beginning. Premature babies don’t know how to “suck, swallow and breathe” all at the same time which is something that an averagebaby would know. The first thing I learned is you had to bottle feed a premature baby.
You had to learn how to hold the premature baby, which is having her to layalong one of my arm, with the other hand holding the bottle and with the rug around her neck. They didn’t know how to suck, swallow and breathe at the same time so constantly, the milk would spill out of their mouth. So I had to learn how to hold the bottle and grab the rug at the same time to dry their mouths.
The next thing I learned is something they call “desat”, which is short for desaturation. Premature babies, for some reason, I don’t know why, they just hold their breaths until they lose oxygen and they could actually die from it. In that case, we had to learn how to stimulate them, rub their bodies just to get them to wake up. Otherwise, they go into a coma. We had to learn to look for signs on their faces - when it turns blue, this is when you have to startto stimulate them.
CHRISTINE STEWART-FITZGERALD: that just sounds really scary.
JULIE KREMRAI: Yes. It’s a whole journey.
CHRISTINE STEWART-FITZGERALD: Sounds like you had to really be able to watch and observe and look at different signs for their health and be aware of a lot of nuances that maybe, let’s just say some parents, who their babies didn’t spend time at NICU—we wouldn’t even be thinking about. Now I’m wondering, on the home front, when you were able to take them home, did you have any assistance? And the caregivers—I’m assuming you probably had to teach, if you did teach them as well what to look for. Julie, how about you?
JULIE KREMRAI: I did not have any assistance initially, except for my husband. We took turns a lot of times in the beginning. Eventually, when we did hire a part time nanny, she went through the whole training of how to take care of premature babies.
CHRISTINE STEWART-FITZGERALD: That is really a real specialty-niche. Suzie how about you? I got to think: just triplets alone require some assistance. How did you do it?
SUZIE DEGWENN: It’s funny. It’s the present tense. We’re living this transition. We’ve only had all three home for about three weeks now. We have gramps. The same people visiting us in the NICU are the same people that are giving us an extra hand here at home. The great thing about that is the nurses were able to teach us a lot in that NICU environment and then that’s transferred here.
One of the best pieces of advice that we got in the NICU—and when I say we, I mean collectively. I mean the grandparents, my husband, myself—is don’t pay so much attention to the monitors. Julie’s point earlier about knowing when your baby turns blue, I tell you that’s not good for their breathing. You’ve got to know what that looks like. And I know for myself atleast, early on in that NICU stay, I was very, very focused on the numbers on the monitors. I really had to consciously look away from that and really get to know what are these cues that my babies were giving me. That made a lot more confident to bring them home.
CHRISTINE STEWART-FITZGERALD: Definitely. Now, we’re going to take a break and when we come back, we’re going to talk about managing that transition with the kids at home and in the NICU because I know you’ve got an older one. We’ll be right back.
Hey Twin Talks. Do you know you can listen to our episodes anytime, anywhere? Just download our apps available on iTunes, Amazon, and Google Play. It’s a great way to listen on the go. Like when you’re waiting for your perinatalogist, or perhaps your twin’s paediatrician. If you want to more great content about twins, be sure to join our Twin Talks Club. You’ll get extra bonus content, transcripts of the shows, discounts on great twin products, and more.
Be sure to visit us online at www.newmommymedia.com .
[Theme Music]
CHRISTINE STEWART-FITZGERALD: Welcome back. Today we are talking with our panellists about bringing home your twins from the NICU. Suzie, we know in your case, that you had two of your triplets—you came home, one in the NICU and you had an older one at home. I’m just imagining. How did you manage all of that?
SUZIE DEGWENN: Oh it’s a circus. My son is two years old and he wasn’t allowed to visit the NICU during those two months that the babies stayed there because in our NICU atleast, he had to be 5 or above. We would read him books about being a big brother. We would say his brothers’ and sister’s names during bed time prayers and supper prayers. But outside of that he really did not know his life was going to change. And of course we’ll bring these two babies home. And then a week later, we bring another baby home.
He’s not happy. If one more person tells me to let him be a helper and hand me a diaper, I think I’m going to scream. Because that’s cute in theory but it doesn’t make him like the babies anymore. I think he’s doing what a two-year old does. He’s regressing a little bit. He’s getting upset when he walks into the baby area and he sees: they’re still here. We’re doing of course our best to give him attention.
We actually did get him a doll. When our hands are full, because there’s just my husband and I. when we’re lucky, we get help for the day. That’s man to man because we’ve got three babies. Christian has his own baby doll that he can burp or feed with a bottle. That actually is going well so far. Much more so than letting him hand me the baby wipes. It seems to frustrate him more. Everybody’s talking advice: let him hand you the diaper.
CHRISTINE STEWART-FITZGERALD: I think that’s a lot of responsibility to put on to a two year old to say: you’re going to be the big brother, you’re going to have to help out. It’s like “what?”
SUNNY GAULT: Especially if they don’t want them there right now. “Let me help you help them—that’s what I want to do” right?
CHRISTINE STEWART-FITZGERALD: Julie, in your case, your girls came home at the same time. Thankfully, you didn’t have to worry. It’s just going home and to the NICU and back and forthwas enough of in itself so we don’t have to worry about the multiple kids. Having kids in the NICU is enough to handle.
Once you got your babies home, or the time period when you knew, okay we’ve got to go ahead, how did you set up your home? Did you have any specific instructions from the NICU staff in terms of what sort of layout you should have at home? Let’s look at the different areas at home. Let’s say the nursery, did they have any specific recommendations for sleeping arrangements, whether they should be in your room or in their own nursery? Should they be in a regular crib or a basinet? How did that work? Julie, how about for you?
JULIE KREMRAI: what I did, which I highly recommend to any parent who has multiple kids—the back of our house was the kitchen, the family room and the nook area, all connected in one big room, and free my shed where I set up shop. I was keeping the same feeding schedule as in NICU for the babies so they didn’t feel any different as far as that went. I set up their bed in the nook area, the dresser for all their clothes. The family room is where they play, and the kitchen is where the food was.
CHRISTINE STEWART-FITZGERALD: So you kept everything altogether. So rather than putting them in a bedroom of their own, off in another corner of the house, it sounds like you centralized everything to keep them close to you where you needed to be.
JULIE KREMRAI: Yes and it was actually to make it easier for me. At night I pretty much sleep on the couch so I was only three feet away from them if they needed anything. Again, I didn’t have a whole lot of help so that was the best situation for me. Eventually I did get some help just so that I could get some sleep. But regardless I just I feltlike that was the best set-up. If I would have to do it all over again and thank goodness I would not have to, that’s what I would do.
CHRISTINE STEWART-FITZGERALD: Right. Suzie, how about for you? Of course you’ve got three of them.
SUZIE DEGWENN: you know what though, great minds think alike because similar to Julie, we had set up shop in a central living area. For us it’s our dining room. What used to be our dining room is now a baby area. We got basinets. Our babies have pretty bad reflux as most primmies do. They’re sleeping right now in rocking place.
I asked the neonatologist specifically, am I winning the bet on this, letting sleep on the rocking place? And they told me early on, basically I cannot train them to sleep either way, you could have the best intentions for sleep training but it’s not going to do me any good. And similarly, it’s not necessarily going to make them never sleep in the crib.
Again, keep in mind, my babies are just only a couple months old. Eventually we will transition them to basinets. Right now we are really just adhering to that NICU feeding schedule and making sure that they get their good rest, which just happens to be in those rocking place that are at an incline. It is a lot much easier for their bellies and digesting their food.
CHRISTINE STEWART-FITZGERALD: Right. How about for you, your sleeping? It sounds likeJuliesaid she wants to be close by the baby. Do you actually get to sleep in your own bed or you’re also out in the common area?
SUZIE DEGWENN: We do shifts here. We have the grandparents with us, sleeping in our guest bedroom pretty much since the babies were born but especially now that they are home. With three babies, we find it’s much easier rather than dividing and conquering. We find it’s easier for two people to feed babies. I’m not nursing, I’m pumping instead so it’s great because everybody can bottle feed the baby.
Two of us, basically, we get one shift off per night because they’re still feeding every three hours and one person just takes the couch after that shift. So I’m sleeping on a combination of my bed and when it’s my shift I sleep on the couch.
SUNNY GAULT: that’s like a well-oiled machine you got going on there Suzie. That’s really smart. That’s organized. You mean business.
SUZIE DEGWENN: I’ve been asked, what happens when the grandparents comes home? And to that I say and I’ve done. Then I go and start calling out these savers and people say, tell me how I can help. You can spend the night and take a shift.
CHRISTINE STEWART-FITZGERALD: I’m imagining you have a chart somewhere with their timeslots, where they will be sleeping
SUZIE DEGWENN: We actually do have a chart. We have a clipboard with each baby’s name at the top, when they last ate and how much they ate because we have already mixed the babies up at this point. I mean they all look alike when they’re all swaddled up at night with hats on and in the dark right?
CHRISTINE STEWART-FITZGERALD: that’s true. I myself did get my girls mixed up one time. Just that one time.
SUNNY GAULT: and I did too. That’s a normal thing and I can imagine if you’ve got three, it’s even harder to do that.
SUZIE DEGWENN: what’s great about that chart too though is if someone wants to help at any time during the day, they can walk over to that clipboard and look and see who ate last, how much they ate, and they can jump into our schedule with us. I guess we kind of set it up selfishly so we could have some help as well.
SUNNY GAULT: productively too. Yes. That’s smart.
CHRISTINE STEWART-FITZGERALD: lastly talking about sleeping, did you guys try to maintain the same schedule in the NICU in terms of sleeping and feeding? Or did it change very much? How about Julie?
JULIE KREMRAI: When we just brought them home. We follow the every three hour schedule just like in NICU. I did not change anything and part of that is that’s the only thing I knew. Once they reached the three, four months gestational of age, not birth age, gestational age which is counting from the time that they were supposed to be born. Not the time that they were born. I started to wean them overnight. I would do the same NICU schedule during the day. But by 9:00, I cut it off and I just let them wake up when they wake up overnight. I was hoping that over time, each period of their sleep would be longer and longer and that’s what happened and then eventually they slept overnight.
CHRISTINE STEWART-FITZGERALD: I was thinking, Suzie, you’re kind of in the mix of it all. Are you pretty much just going by the NICU schedule?
SUZIE DEGWENN: Yes. I think I would be a big dummy if I didn’t. Because one of the hardest thing to do is to get a baby into any set schedule. So our babies, in terms of feeds in the NICU, one at the top of the hour, one at the half hour, one at the top of the hour again. And that’s what we maintained here. There are about three hours, four hours apart between feeds. But we’re still in the order that they were in the NICU.
There have been times that we’ve have woken the babies up to feed them. In my head, I would think, “oh you big dummy. Why would you wake a sleeping baby. But I wake the sleeping baby because they’re on that schedule. If I let that baby sleep until whenever they feel like getting up, like right now, that means I’m always feeding the baby, like all the time.
Because when we’ve got two people on our shift, it probably takes us an hour or an hour and a half through the feedings.When they’re feeding every three hours, you see how that could get really messy if you just let the baby take the reign.
CHRISTINE STEWART-FITZGERALD: And plus you’re pumping. That’s a huge time consideration in itself. My hat is off to you. I want to say thank you to both of you for joining us today. For everyone, be sure to visit our episode page and our website for more information about our series: Inside the NICU as well as links to additional resources. And this conversation continues for members of our Twin Talks Club. After the show, we’ll talk about creative ideas for NICU caregivers.
For more information on the Twin Talks Club, visit our website, www.newmommymedia.com
[Theme Music]
SUNNY GAULT: Hey Twin Talks. It’s time for our special segment on the show we like to call Special Twin Moments. This moment comes from Jillian. Jillian posted this to the Multiples of America Facebook page. We were actually on there recently and we’re asking you guys to submit your special twin moments. Here’s what Jillian had to say:
The first time my son laughed, a big, deep belly laugh, was when he was about three months old and laying on the bed with his twin. They were holding hands and babbling to one another. He grabbed his brother by the hand, looked into his eyes and let out the sweetest, funniest laugh I’ve ever heard.In that instant, I realized how strong their bond was. And it is still today at six years old. I will always remember that moment as the sweetest in my life.
---Jillian
Oh I love this. I can just picture all of this happening. Jillian, thank you so much for writing this and it was great sharing your special twin moment. If you guys have a special twin moment you want to share with all of our listeners, you can call our voicemail at 619-8664775 and leave us a message and we’ll include your story on a feature episode.
CHRISTINE STEWART-FITZGERALD: So that wraps up our show for today. We appreciate you listening to Twin Talks.
Don’t forget to check out our sister show:
• Preggy Pals for expecting parents
• The Boob Group for moms who breastfeed their babies
• Parent Savers yourparenting resource on the go
• Newbies for postpartum moms thru their baby’s first year
This is Twin Talks, parenting times two.
[Disclaimer]
This has been a New Mommy Media production. The information and material contained in this episode arepresented for educational purposes only. Statements and opinions expressed in this episode are not necessarily those of New Mommy Media and should not be considered facts. While such information and materials are released to be accurate, it is not intended to replace or substitute for professional, medical advice or care and should not be used for diagnosing or treating health care problem or disease or prescribing any medications. If you have questions or concerns regarding your physical or mental health or the health of your baby, please seek assistance from a qualified health care provider.
SUNNY GAULT: New Mommy Media is expanding our line-up of shows for new and expecting parents. If you have an idea for a new series, or if you’re a business, or an organization interested in joining our network of shows through a co-branded podcast, visit www.NewMommyMedia.com.
[00:36:31]
[End of Audio]